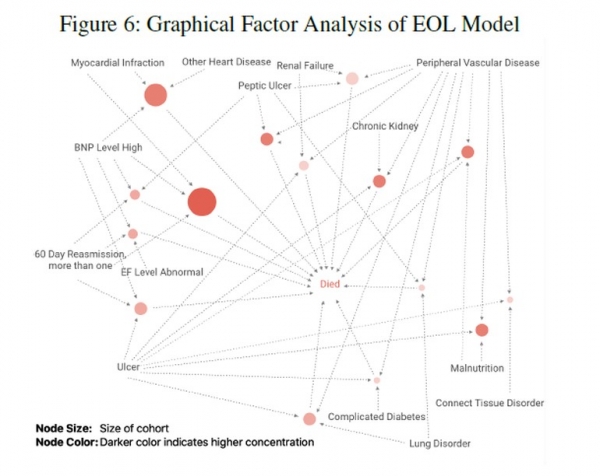
KenSci, a company that develops a machine learning risk prediction platform for the medical industry , recently published a paper on predicting dying mortality and improving care. This paper is aimed at a very difficult topic, predicting the patient's risk of death in the last six to twelve months, and it has been accepted by the Association for the Advancement of Artificial Intelligence. At a critical juncture, $205 billion spent on nursing in the last year of personal life. But this is not just a matter of cost. The following is an excerpt from the paper "Death vs. Data Science: Predicting End of Life." The number of Americans using palliative care services continues to grow, with an estimated 1.7 million people, or 46% of deaths (NHPCO 2016). However, these services were used too late: in 2016, the median duration of stay in hospice hospitals was only 23 days. In addition, 28% of hospice patients were discharged or died within 7 days of admission (NHPCO 2016). In the work of Christakis and colleagues, they believe that hospice physicians feel that 80-90 days of hospice care is best suited to the needs of patients and their families (Christakis 1997). A survey of family members of the deceased showed that satisfaction with hospice care was related to their perception of the timeliness of hospice referrals (Teno et al. 2007). Finally, among the medical institutions that often experience the death of inpatients, the proportion of burnouts among health care workers such as emergency medical care providers and intensive care nurses is very high (Embriaco et al., 2007). Therefore, the final conclusion is that timely and appropriate hospice care affects all aspects of Quadruple Aim's healthcare (quality, satisfaction, cost savings and provider satisfaction). We are organizing a series of articles about data scientists and the methods they use. As part of this series, we "caught" KenSci's chief technology officer and one of the authors of the paper, Ankur Teredesai, in this paper. Recognized in emerging technology categories. What data set do you use to model? Predicting the risk of mortality within six to twelve months is a very complex challenge. In the United States, this is a question worth $205 billion. At KenSci, we have a platform designed to increase the scale and operational efficiency of machine learning to address such issues with enormous social impact. In this particular environment, we have a machine learning model that predicts mortality within six to twelve months based on previous efforts. We worked with two major medical systems in the Northwestern United States and retrained our models and created more models with new data. Data from Health System A contains a population of patients with a history of heart failure (HF), including 4,888 patients, and their various electronic medical record data, including: Demographic characteristics Length of time the patient stayed Overall cost related characteristics Re-admission information for specific cost-related characteristics (inpatients, outpatients, family health, hospice care, skilled care facilities) Tracking the executed program through the Healthcare Common Procedure Coding System (including ambulances, Medical Equipment , prosthetics, etc.) Health System B's data includes 48,365 patients with various types of illnesses. Health System B only has medical claim data available. This paper details the data elements used for modeling. How is big data technology applied to your research? What kind of dream data sets are missing from this work? We used Microsoft's Azure cloud to run some of the underlying components. We also seamlessly integrate with existing enterprise big data investments to ensure that the healthcare industry can benefit from a wide range of data sources. KenSci has partnered with healthcare partners around the world to collect data sets from EMR ( Electronic Medical Records), social psychology data, medical claims and financial information to achieve patient and overall hospital population status. Longitudinal observation. The system is cloud-based, so you can connect to new data sources as they become available. Forecasting the mortality rate of six to twelve months and helping doctors turn patients into palliative care based on the insights obtained, the prediction in this case is a very complicated task. Data such as demographics and comorbidities provide good results, but additional data sources such as changes in doctor input or prescription often provide additional information. After all, there has never been an ideal "dream" dataset in machine learning. The information contained in the EMR about a patient tends to be less than 10%. In an increasingly connected world, we will continue to generate additional data assets, increasing the complexity of data-driven decision making. The advantage of machine learning is the ability to learn step by step and improve with more data and feedback. How did you build this model? What role does human input play in building it? We have built a model with assistive intelligence in our minds. Every model we develop at KenSci is based on the idea that human input will be a key factor in every step of the care. The KenSci Machine Learning (ML) platform facilitates interpretable machine learning models that explain their correctness and validation, and then KenSci's doctors and clinicians not only validate the output of the machine learning model, but also help determine clinical work. The input features in the stream are then integrated into any tool. The whole process is very strict, and we are always looking for ways to make it more complementary, while still being rigorous. This topic is a very sensitive topic, and there are naturally concerns about using algorithms to determine care. What method is best used to determine what care should be taken during hospice care? At KenSci, we are committed to improving the quality of patient outcomes by increasing the efficiency of hospitals and caregivers. Using artificial intelligence algorithms can provide insights into who may get sick, how to get sick, when to get sick, and how to effectively serve patients throughout the duration of care. While artificial intelligence is still a newcomer to healthcare, its intelligence can be used by caregivers and hospital systems to increase efficiency. The doctor is always the decision maker, and the algorithm does not interfere with the relationship between the doctor and the patient. Broad sense of intelligence is a tool we need to use, but when it comes to health care and dying problems, the decision is in the hands of doctors and patients. At KenSci, we see artificial intelligence as a secondary intelligence, which is designed to help experts who are using the technology, not to replace them. This also applies to the issue of hospice care discussed here. These models are designed to help doctors notice attributes that may be neglected, because machine learning can pay attention to a large number of variables in stratification, so artificial intelligence can provide additional knowledge to make more informed decisions. Is it possible to study without EHRs? How do you deal with unstructured data in the medical system (ie data on paper or something worse)? EHR data is necessary but not sufficient to generate insights and predictions in the medical field. Although unstructured data can add useful additional information to the predictive model, even simple problems in the medical system remain unresolved, because even structured data has not yet played their full role. Structured data provides sufficient richness to provide descriptive statistics and provide adequate predictive models for re-admission risk, mortality prediction, and emergency department utilization estimates. However, EHR and other structured data have not yet reached their full potential. These predictions are essentially different from person to person. So, how do you deal with topics like cost savings at the macro level? Although hospice care is inherently personalized, predicting high-cost patient cohorts and identifying patterns that result in high costs and high utilization are critical to hospitals and health systems. KenSci's solution can help identify high-cost populations by analyzing longitudinal medical records, improving the utilization of palliative care by modeling disease and predicting end-of-life outcomes to predict future high-volume populations. However, a system like this can do more than just provide a life endpoint prediction – it also allows healthcare professionals to explore the patient's risk profile and predict potential re-admission possibilities. While cost reductions are clearly attractive for medical systems, such systems can also provide better care for patients in all areas. In all cases, machine learning systems can help reduce the doctor's burnout and assist in the configuration and presentation of patients who may need medical intervention. Insights gained from machine learning systems can help caregivers to engage with more informed and motivated communication about their customers' desire for hospice care. ZHEJIANG SHENDASIAO MEDICAL INSTRUMENT CO.,LTD. , https://www.sdsmedtools.com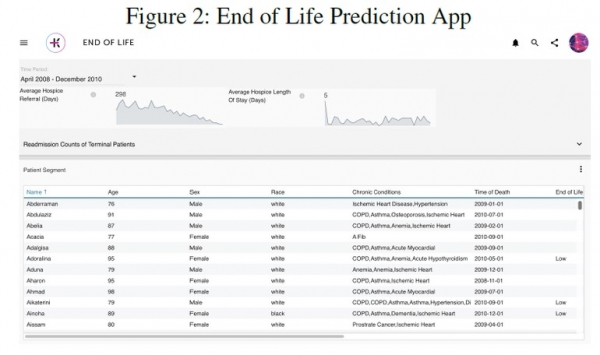
Death and Data Science: See how machine learning can improve hospice care
Next Article
Spare parts PLC system 1756-IF16 input module
Prev Article
Portable Shr Hair Removal Opt IPL Beauty Machine